Abstract
Background: Electronic consultation (e-consultation) refers to asynchronous electronic communication between a consulting provider and a consulted specialist. Recommendations are formulated by medical record review and communicated via medical record documentation without direct contact between the specialist and patient.
There is a current shortage of non-malignant hematologists and hence a need to optimize the efforts of the existing workforce. E-consultation holds promise by allowing simpler consults to be answered quickly, reserving face-to-face (FTF) encounters for complex hematologic questions and therefore allowing hematologists to serve a larger number of patients. Additional benefits of e-consultation include faster response to consultation questions and decreased travel burden for patients.
However, due to lower financial incentives for e-consultation compared to FTF in fee-for-service reimbursement models, adoption has been limited. Here, we report the experience with e-consultation in non-malignant hematology in a fee-for-service model at a large academic medical center and compare that experience to published reports in three medical centers with non-fee-for-service models.
Methods: On March 1, 2021, the outpatient clinic of the University of Alabama at Birmingham (UAB), implemented e-consultation for non-malignant hematology. E-consults could be initiated by any provider within the UAB system through electronic order entry. Three non-malignant hematologists reviewed and responded to all e-consults and these hematologists, along with an advanced practice provider, conducted all FTF encounters.
Retrospective analysis of e-consultation practices, 1 year after implementation was performed. Variables collected included the reason for consultation, date and time of response, the time between e-consult and response, time to review and respond, frequency of conversion to an FTF encounter, and follow-up communication.
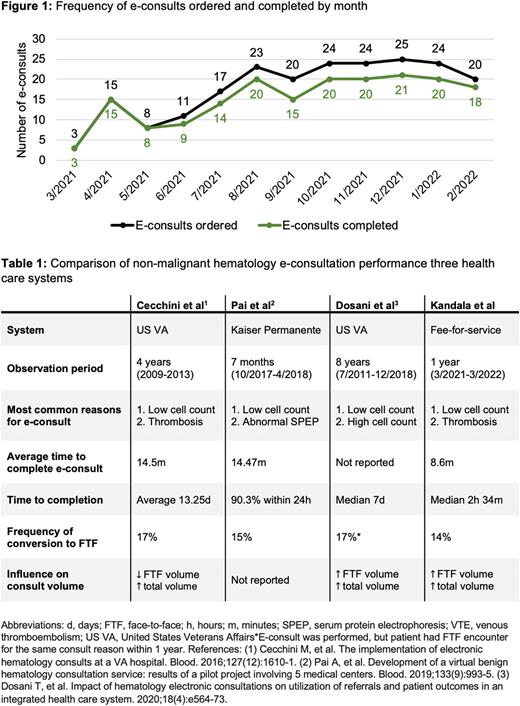
Results: Over the 1-year study period, 214 e-consults were requested, of which 183 (86%) had an e-consult completed and 31 (14%) were converted to an FTF encounter due to complexity. The frequency of e-consults ordered and completed (i.e., not converted to an FTF encounter) by month is presented in Figure 1.
The most common diagnoses prompting consultation included anemia (21%), thrombosis (19%), leukopenia (12%), and thrombocytopenia (11%). There was more than one diagnostic question in 29 e-consults (14%).
The average time to review and respond to an e-consult was 8.6 minutes (range 2-20 minutes). The median time from the e-consult request to completion was 2 hours and 34 minutes (IQR 9 hours and 46 minutes). Additional workup, including laboratory testing and/or imaging, was recommended in 56% of e-consults and was performed by the consulting provider. Subsequent communication between the consulting provider and non-malignant hematology provider within 30 days of the e-consult was required in 13% of e-consults.
The total number of FTF new patient encounters scheduled in the study year increased to 2,642/year from 1,708/year in the year before e-consult implementation. The average wait time for a physician FTF new patient appointment also increased from 56 days to 88 days.
Table 1 presents a comparison of the performance of reported e-consultation systems in non-malignant hematology. Low cell counts (anemia, thrombocytopenia, and leukopenia) were the most common reason for consultation in all systems. Our e-consult system demonstrated a shorter time to complete the consult and a shorter time to respond. A consistent percentage (14-17%) of e-consults were converted to FTF encounters. In the two programs that measured influence on consult volume, both reported a similar increase in total consult volume after e-consult implementation.
Conclusions: In a large fee-for-service medical center, the implementation of e-consultation for non-malignant hematologic care did not decrease consult volume, and consulting provider uptake was low. However, when used, e-consultation facilitated rapid delivery of non-malignant hematologic expertise and performed similarly to reported experiences in non-fee-for-service models. Further investigation is needed to determine how e-consultation can be best utilized to maximize access to expertise in non-malignant hematology.
Disclosures
Gangaraju:Alexion: Consultancy; Sanofi Genzyme: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal